
blog detail
August 4, 2025
Telemonitoring
Heart failure (HF) remains one of the most challenging chronic conditions for healthcare systems globally. In New Zealand alone, thousands of people live with heart failure, many of them older adults, rural residents, and vulnerable populations who face additional barriers to care. One of the most critical phases in managing HF is the up-titration of guideline-directed medical therapy (GDMT), a process that involves gradually increasing medication doses to reach optimal levels for each patient. The evidence is clear: when patients achieve target doses of GDMT faster, they experience better quality of life, fewer hospital admissions, and improved survival.
Yet in practice, many patients never reach these target doses. Traditional models of care, reliant on in-person clinic visits and manual follow-up, are too slow, too resource-intensive, and too inaccessible for the scale of need. That’s why it’s time to make the rapid titration of GDMT for HF patients "digital by default."
Digital by default means using remote patient monitoring (RPM) and virtual care tools as the first-line approach to titration—reserving in-person care for cases where it's clinically necessary. With the right digital infrastructure in place, we can redesign titration pathways around real-time patient data, virtual consultations, and streamlined clinical workflows that allow for fast, safe decision-making from a distance.
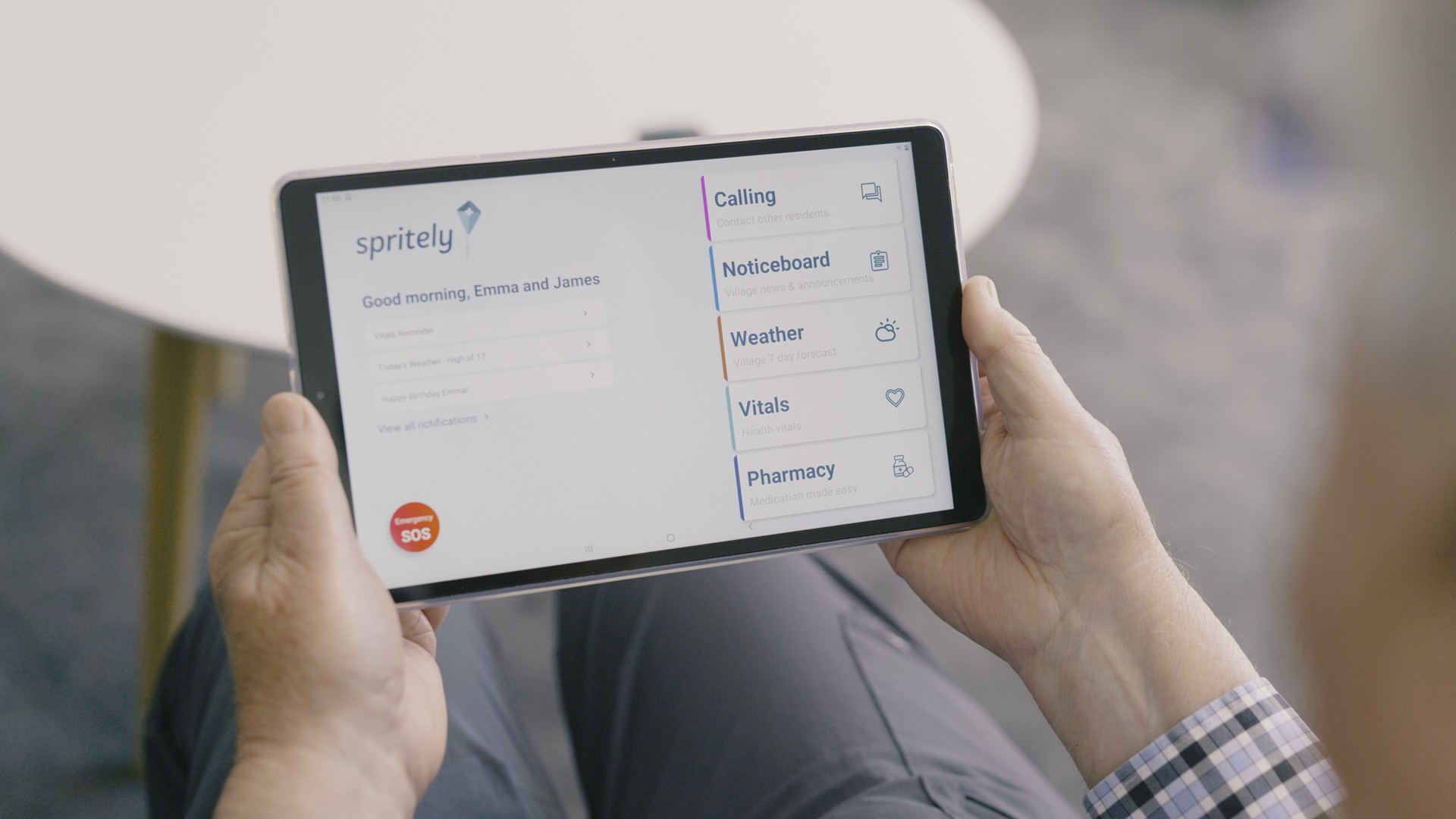
This model doesn’t eliminate the human connection or clinical oversight—it enhances it. Patients are still supported by nurses, pharmacists, and cardiologists. But instead of traveling back and forth to clinic for months, they measure their vital signs from home, report symptoms through a dedicated tablet, and connect with their care team virtually.
In Hawkes Bay, where a digital RPM model for rural HF patients was piloted, patients achieved optimal GDMT doses in just 6–8 weeks. That’s a dramatic improvement from the 6–8 months it typically takes under standard care. Faster titration means patients get the full benefit of life-saving medications much sooner.
By closely monitoring weight, blood pressure, oxygen saturation, symptoms, and having more frequent video-enabled consults, clinicians can detect decompensation early and intervene before a hospitalisation is required. In Hawkes Bay, the 30-day readmission rate for patients managed with digital RPM was 0%, compared to 25% in the standard care group.
Digital workflows allow cardiac nurses to oversee more patients without compromising care quality. Vital sign alerts and symptom trends are summarised on a dashboard, enabling quick triage and follow-up. The time saved on travel, appointment admin, and DNA minimisation can be reinvested into clinical decision-making and proactive care.
Patients benefit from care that fits into their lives. No more taking time off work, finding transport, or sitting in waiting rooms. With digital titration, they are actively involved in their own care, supported by technology that is designed to be easy to use—even for those with no prior digital experience.
Each patient managed through the digital model in Hawke’s Bay saved the system an average of $9,500. These savings come mainly from reduced hospital stays and fewer in-person appointments. Over time the health system saves even more because heart failure patients who receive GDMT experience more years free from hospitalisation due to heart failure. When scaled, this model has the potential to save tens of millions annually across New Zealand and hundreds of millions over the following decades.
Digital-first models can also close the equity gap in heart failure care—if designed properly. Devices must be pre-configured, data-enabled, and easy to use so that patients don’t need to supply their own phones, data, or technical knowledge. Spritely RPM device kits were co-designed with older adults, making them accessible even to those who have never used a touchscreen before.
By removing barriers to participation—such as distance, mobility, or digital access—digital titration becomes not just a more efficient way of delivering care, but a more inclusive one.
It’s time to reimagine how we deliver high-value care for chronic conditions like heart failure. Making rapid titration of GDMT "digital by default" does not replace clinicians—it equips them with better tools to do their jobs more efficiently and effectively. It’s about freeing up hospital space, reducing wait times in ED, and giving more patients optimal care.
We’ve seen that this approach works. It delivers faster titration, better outcomes, and significant savings. The next step is to scale it.
At Spritely, we’re committed to supporting this transition. Our platform is built to support digital titration at scale—securely, reliably, and equitably. With the right partnerships we can help make digital-first titration the new standard for heart failure care in New Zealand and beyond.
Interested in learning how digital titration could work in your region? Get in touch with the Spritely team to find out more.

October 28, 2025

September 16, 2025